Hyperthyroidism in Cats
Cats have 2 thyroid glands located in the neck on either side of the trachea. The thyroid gland produces thyroid hormones, crucial for regulating the metabolism of most of the organs in the body. In other words, the thyroid hormones control how fast the organs work.
Hyperthyroidism is caused by an increased production of thyroid hormone (thyroxine – T4) from an overactive thyroid gland. In the majority of the cases (98%) hyperthyroidism is linked to benign (non cancerous) changes in the gland. In some rare occasions (<2%) the disease can be linked to malignant cancer.
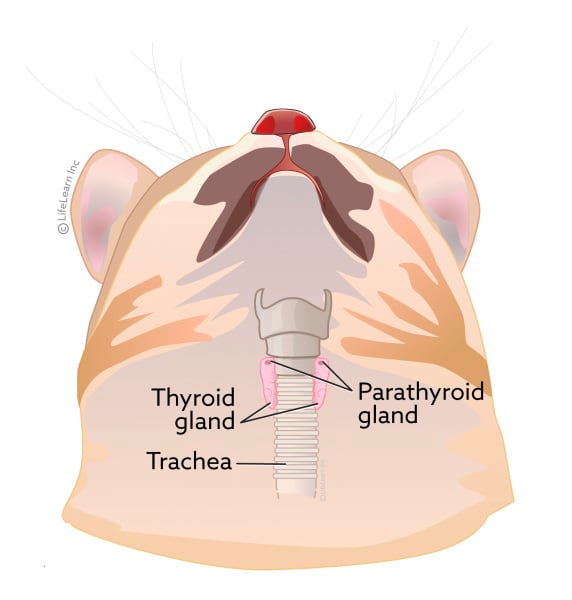
Image from: https://vcahospitals.com/know-your-pet/hypocalcemia-or-low-calcium-levels-in-cats
WHAT ARE THE SIGNS OF HYPERTHYROIDISM?
Initially, the signs can be mild, but they can become more severe as the disease progresses. The most common signs observed are weight loss, increased appetite, increased water intake, hyperactivity, increased heart rate, heart murmur, diarrhoea, vomiting, and heat intolerance. On the other hand, as thyroid hormones control the body’s metabolism, their rise could cause secondary complications in other organs or mask underlying diseases that might require further investigation.
- Heart → high T4 levels can cause an increased heart rate and heart contractions. In order to meet those demands, the heart enlarges, which might eventually lead to cardiac failure and potentially death. Usually, cardiac signs improve once hyperthyroidism has been controlled.
- Hypertension → increased T4 can cause hypertension. High blood pressure will impact other organs such as eyes, kidneys, heart, and brain. Initially, the patient might need medication to control the blood pressure; however, if hyperthyroidism is well controlled, eventually, the medication used for hypertension could be discontinued.
- Chronic kidney disease (CKD) → while CKD is not caused by the direct impact of thyroid hormones, usually, both diseases coexist in geriatric cats. Hyperthyroidism tends to increase the blood flow to the kidneys, which gives the false impression that the kidneys are working properly (the blood results might show normal kidney values as increased T4 is masking kidney disease). However, successful treatment for hyperthyroidism might lead to a decline in renal function (abnormal values observed in blood and urine tests)
HOW IS HYPERTHYROIDISM DIAGNOSED?
- Palpation of the thyroid gland → In some cases, your vet might be able to feel the thyroid gland during the physical examination. It might feel like a small firm mass in the neck; however, this is not evident in every patient.
- Blood test
- T4 → elevation of T4 levels above normal limits will confirm the disease. This measurement is also useful as a screening test for monitoring treatment.
- Free T4 (FT4) → FT4 is the non-protein-bound T4 present in the blood. Your veterinarian might recommend measuring FT4 in cats with high borderline T4 levels in order to confirm the disease.
- Thyroid Stimulating Hormone (TSH) → this test can be used in combination with the other thyroid tests mentioned above. Hyperthyroid cats will generally have low levels of TSH.
TREATMENT
There are different treatment alternatives for hyperthyroidism. Each one of them has its advantages and disadvantages. To choose the right treatment for your pet, we might consider certain factors like the age of the cat, existing medical conditions, and the cost of the treatment. The treatment options for hyperthyroidism are:
- Oral medications used to reduce the production of T4
- Pros:
- The drugs are usually effective with a low risk of secondary effects
- Low cost initially (in the long term, it might be as expensive or even more expensive than other treatment alternatives)
- No hospitalization is required
- Cons:
- The medication usually needs to be administered daily for life.
- This treatment doesn’t cure the disease but allows its control as long as the medication is used.
- The dose used might need to be adjusted as the disease advances, thus blood tests will be required to evaluate the efficacy of the treatment and dose adjustments.
- Once a patient is stable, periodical veterinary monitoring and blood tests should be repeated every 3- 6 months.
- Not considered a curative treatment
- Pros:
- Surgical treatment → removal of the thyroid gland(s)
- Pros:
- Usually leads to a permanent cure
- No further treatment is required unless complications arise
- Cons:
- In some cases, the disease might return if part of the tissue is left behind.
- The procedure requires general anesthesia
- Possible damage to the parathyroid glands (small glands close to the thyroid) can happen during the procedure. Parathyroid glands are crucial to maintain normal calcium levels in the blood, therefore damaging them can be life-threatening if not addressed properly.
- Pros:
- Radioactive iodine (I 131) → This is administered via injection. The iodine is selectively taken and destroys abnormal thyroid tissue without damaging healthy organs.
- Pros:
- Considered the gold standard treatment for hyperthyroidism
- Usually leads to a definitive cure (95% success rate)
- Secondary effects are unlikely
- The process doesn’t require general anesthesia
- Usually, pharmacological treatment is not required after the procedure.
- Cons:
- Patient needs to be isolated for about 1 week → Radioactive material is not a risk for the patient but it can be dangerous for the people around them. It is for this reason that the treatment needs to be done in special facilities, and patients need to be hospitalized until the radioactivity levels have decreased to acceptable levels.
- Relatively expensive compared with other treatment options
Follow-up blood tests are recommended after the procedure to evaluate efficacy of the treatment during the first year after treatment. - In <5% of the cases the cat might become HYPOthyroid after the treatment. In which case daily oral medication will be required
- Pros:
- Diet (Hill’s Y/D) → this treatment consists of exclusive feeding of a special diet that has strictly low levels of iodine (normally used by the thyroid gland to make more thyroid hormone).
- Pros:
- This therapy has been successful in some patients (> 80% response rate)
- Only change of diet is required.
- Safe in cats with other diseases
- Cons:
- The cat is not allowed to consume anything else for the rest of their lives. Relapse rate 100% when off the diet.
- Not considered a curative treatment.
- Relatively expensive compared to regular cat food
- Pros:
Overall, cats respond well to treatment for hyperthyroidism, and if the disease is well controlled, the patients usually have a good prognosis and quality of life. Currently, there are no known ways to prevent this disease; however, an early diagnosis decreases concurrent damage to other organs and increases the prognosis of the patient. If you suspect that your middle-aged/senior cat might be showing possible signs of hyperthyroidism or if they’re due for annual blood work, please don’t hesitate to contact us.


